Endometriosis is a chronic gynecological condition that affects millions of women worldwide. Characterized by the presence of endometrial-like tissue outside the uterus, it leads to symptoms like chronic pelvic pain, dysmenorrhea, and infertility. Recently, researchers have begun to explore a potential link between endometriosis and autoimmune diseases, shedding light on why some women experience more severe forms of this condition. Understanding this connection is crucial for better diagnosis, management, and treatment.
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterine cavity. These growths, known as lesions, can appear on the ovaries, fallopian tubes, and the pelvic lining. This ectopic tissue behaves like normal endometrial tissue—it thickens, breaks down, and bleeds with each menstrual cycle. However, because this blood has nowhere to go, it leads to inflammation, pain, and the formation of scar tissue.
Endometriosis affects approximately 10% of women of reproductive age. Common symptoms include severe menstrual cramps (dysmenorrhea), chronic pelvic pain, pain during intercourse, and infertility. Some women may also experience gastrointestinal issues, fatigue, and heavy menstrual bleeding.

Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues, considering them as foreign invaders. This leads to chronic inflammation and a variety of symptoms depending on the tissues affected. Some common autoimmune diseases include:
The impact of autoimmune diseases can be widespread, affecting various organs and systems and significantly impairing quality of life.
Recent studies suggest that women with endometriosis are at a higher risk of developing autoimmune diseases. This association may be due to shared immunological and inflammatory pathways. For instance, both conditions involve chronic inflammation and immune system dysregulation. Research indicates that the prevalence of autoimmune diseases such as SLE, RA, MS, and others is higher in women with endometriosis compared to the general population.
Women with endometriosis have been found to have an increased risk of developing SLE, a complex autoimmune disease that affects multiple systems in the body.
The chronic inflammation associated with endometriosis may contribute to the development of RA, characterized by painful and swollen joints.
MS, a condition that affects the central nervous system, has also been linked to endometriosis, suggesting a possible shared inflammatory mechanism.
SS primarily affects the glands that produce saliva and tears, leading to dry mouth and eyes. Women with endometriosis may be more prone to developing SS.
Conditions like Hashimoto’s thyroiditis and Graves’ disease, which affect thyroid function, are more common in women with endometriosis.
CLD, an autoimmune disorder triggered by gluten consumption, has been found to have a higher prevalence in women with endometriosis.
IBD, which includes Crohn’s disease and ulcerative colitis, involves chronic inflammation of the digestive tract and is more frequently observed in women with endometriosis.
Recent research has explored whether autoimmune diseases can influence the severity of endometriosis. A study published in Scientific Reports found that women with both endometriosis and autoimmune diseases were more likely to have stage IV endometriosis, the most severe form of the condition. This suggests that the hyper-inflammatory state common to both conditions may exacerbate the progression of endometriosis.

The connection between endometriosis and autoimmune diseases may be explained by immune system dysregulation and chronic inflammation. Both conditions involve an overactive immune response that leads to tissue damage and inflammation. Additionally, genetic factors and environmental triggers may play a role in predisposing women to both endometriosis and autoimmune diseases.
Women with endometriosis and concomitant autoimmune diseases may require more frequent monitoring to manage the progression of their conditions effectively. Regular check-ups and diagnostic tests can help in early detection and intervention.
Understanding the link between these conditions can help healthcare providers develop personalized treatment plans that address both endometriosis and autoimmune diseases. For example, anti-inflammatory medications and immunomodulators might be beneficial in managing both conditions simultaneously.
Identifying autoimmune diseases in women with endometriosis early on may allow for interventions that could mitigate the severity of endometriosis. Early treatment can help manage symptoms and prevent complications.
Treatment options for endometriosis include pain management with NSAIDs, hormonal therapies to reduce or eliminate menstruation, and surgical interventions to remove endometrial lesions.
Treatment for autoimmune diseases often involves medications to suppress the immune system, reduce inflammation, and manage specific symptoms. These may include corticosteroids, immunosuppressants, and biologics.
Integrative approaches, such as acupuncture, dietary modifications, and stress management techniques, can be beneficial in managing both endometriosis and autoimmune diseases. These approaches aim to reduce inflammation and support overall health.
Living with both endometriosis and autoimmune diseases can take a significant physical and emotional toll. Chronic pain, fatigue, and the unpredictability of symptoms can affect daily activities and mental health. It’s important to develop coping strategies, such as mindfulness practices, support groups, and professional counseling, to manage the emotional impact.
A multi-disciplinary approach is essential in managing endometriosis and autoimmune diseases. This involves collaboration between gynecologists, rheumatologists, immunologists, and other specialists to provide comprehensive care. Personalized treatment plans should address the unique needs of each patient, considering both conditions.
Current research has made significant strides in understanding the link between endometriosis and autoimmune diseases, but there are still gaps that need to be addressed. Future research should focus on the underlying mechanisms, genetic predispositions, and potential environmental triggers. Developing targeted therapies that address both conditions simultaneously is a promising area for future investigation.
Patient stories and experiences can provide valuable insights into living with these conditions. Support networks, both online and offline, offer a sense of community and shared understanding. Resources such as patient advocacy organizations, educational materials, and healthcare provider directories can help women navigate their journey with endometriosis and autoimmune diseases.
No, endometriosis itself does not turn into an autoimmune disease. However, it has been observed that women with endometriosis are at a higher risk of developing autoimmune diseases. This association is likely due to shared immune system dysregulation and chronic inflammation.
2. How are autoimmune diseases diagnosed in women with endometriosis?
Diagnosis of autoimmune diseases involves a combination of medical history, physical examination, and various tests, including blood tests for specific autoantibodies, imaging studies, and sometimes biopsy. Women with endometriosis should inform their healthcare provider about all their symptoms to ensure comprehensive evaluation.
3. What lifestyle changes can help manage both endometriosis and autoimmune diseases?
Lifestyle changes that can help manage both conditions include maintaining a balanced diet rich in anti-inflammatory foods, regular physical activity, stress management techniques such as yoga or meditation, and adequate sleep. Avoiding known triggers and maintaining a healthy weight can also be beneficial.
4. Are there specific diets recommended for managing endometriosis and autoimmune diseases?
While there is no one-size-fits-all diet, many women find relief with anti-inflammatory diets. These diets typically include plenty of fruits, vegetables, lean proteins, and healthy fats while avoiding processed foods, refined sugars, and excessive caffeine or alcohol. Gluten-free diets may be helpful for those with celiac disease.
5. How can I find support if I have both endometriosis and an autoimmune disease?
Support can be found through various channels, including online support groups, local patient advocacy organizations, and mental health professionals. Connecting with others who understand your experience can provide emotional support and practical advice for managing both conditions.
Endometriosis and autoimmune diseases are complex conditions that share many commonalities, including chronic inflammation and immune system dysregulation. Recent research has highlighted the link between these conditions, emphasizing the need for comprehensive care and tailored treatment strategies. Women with endometriosis should be vigilant for symptoms of autoimmune diseases and seek medical advice for appropriate diagnosis and management. By understanding the connection and implementing effective treatment plans, healthcare providers can improve the quality of life for women affected by these challenging conditions.
If you suspect you have endometriosis or an autoimmune disease, it is crucial to consult with a healthcare provider to receive an accurate diagnosis and appropriate treatment.

Endometriosis is a painful condition where tissue similar to the lining inside the uterus grows outside of it, often causing severe pain and complications, including fertility issues. Many women suffer from both endometriosis and difficulties with conceiving. Fortunately, acupuncture and Chinese herbal medicine offer natural, effective ways to alleviate pain and improve fertility outcomes.
1. Enhancing Blood Flow
Acupuncture involves the insertion of thin needles into specific points on the body. These needles help to improve blood flow to the pelvic area, reducing inflammation and pain. Better circulation means that nutrients and oxygen are delivered more efficiently, promoting healing and reducing pain.
2. Releasing Endorphins
When acupuncture needles are inserted, the body releases endorphins, which are natural painkillers. These endorphins help to relieve the chronic pain associated with endometriosis, making it easier to manage daily activities without discomfort.
3. Balancing Hormones
Hormonal imbalances often play a significant role in endometriosis. Acupuncture helps to regulate the endocrine system, which is responsible for hormone production. By balancing hormones, acupuncture can reduce the severity of endometriosis symptoms.
4. Reducing Inflammation
Inflammation is a key factor in endometriosis pain. Acupuncture has been shown to reduce inflammatory markers in the body, leading to less pain and swelling in the affected areas.
1. Anti-Inflammatory Properties
Chinese herbs such as turmeric and ginger have natural anti-inflammatory properties. When used as part of a customized herbal formula, these herbs can help to reduce the inflammation that contributes to endometriosis pain.
2. Pain Relief
Certain herbs, like corydalis, are known for their pain-relieving properties. Herbal formulas can be tailored to target specific types of pain, providing relief from the discomfort caused by endometriosis.
3. Hormonal Regulation
Herbal medicine can also help to balance hormones naturally. Herbs like peony and dong quai are often used to regulate menstrual cycles and reduce symptoms of hormonal imbalance, which can alleviate endometriosis symptoms.
1. Reducing Stress
Stress is a significant factor that can negatively impact fertility. Acupuncture promotes relaxation by stimulating the release of neurotransmitters like serotonin and dopamine. This stress reduction can improve reproductive health and increase the chances of conception.
2. Improving Blood Flow to Reproductive Organs
Acupuncture enhances blood flow to the ovaries and uterus, improving their function. Better circulation means a healthier uterine lining and improved ovarian function, which are essential for successful conception and implantation.
3. Regulating Menstrual Cycles
Acupuncture can help to regulate menstrual cycles, ensuring that ovulation occurs more predictably. A regular menstrual cycle is crucial for timing intercourse or fertility treatments to increase the likelihood of conception.
1. Supporting Ovulation
Certain herbs, such as chaste tree berry (Vitex), support regular ovulation by balancing hormones and regulating the menstrual cycle. This can enhance the chances of conception.
2. Reducing Inflammation
Inflammation in the reproductive organs can hinder fertility. Herbal medicine, with its anti-inflammatory properties, can reduce inflammation, improving the overall health of the reproductive system.
3. Strengthening the Uterine Lining
A healthy uterine lining is essential for the implantation of a fertilized egg. Herbs like raspberry leaf and nettle leaf are known to strengthen and nourish the uterine lining, making it more receptive to implantation.
By combining acupuncture and herbal medicine, individuals can address both the pain associated with endometriosis and the fertility challenges it may cause. This integrative approach provides a holistic treatment that not only alleviates symptoms but also improves overall reproductive health.

Q: Is acupuncture painful?
A: Acupuncture is generally not painful.
Q: How long does it take to see results with acupuncture and herbal medicine?
A: Results vary depending on the individual and the severity of their condition. Expect to be treated for three to six months to improve fertility outcomes and one month to reduce pain.
Q: Are there any side effects to using herbal medicine?
A: No.
Q: Can acupuncture and herbal medicine be used alongside conventional treatments?
A: Yes, acupuncture and herbal medicine can complement conventional treatments.
Acupuncture and herbal medicine offer effective, natural ways to reduce pain associated with endometriosis and improve fertility outcomes. These therapies provide holistic support for better reproductive health and overall well-being.
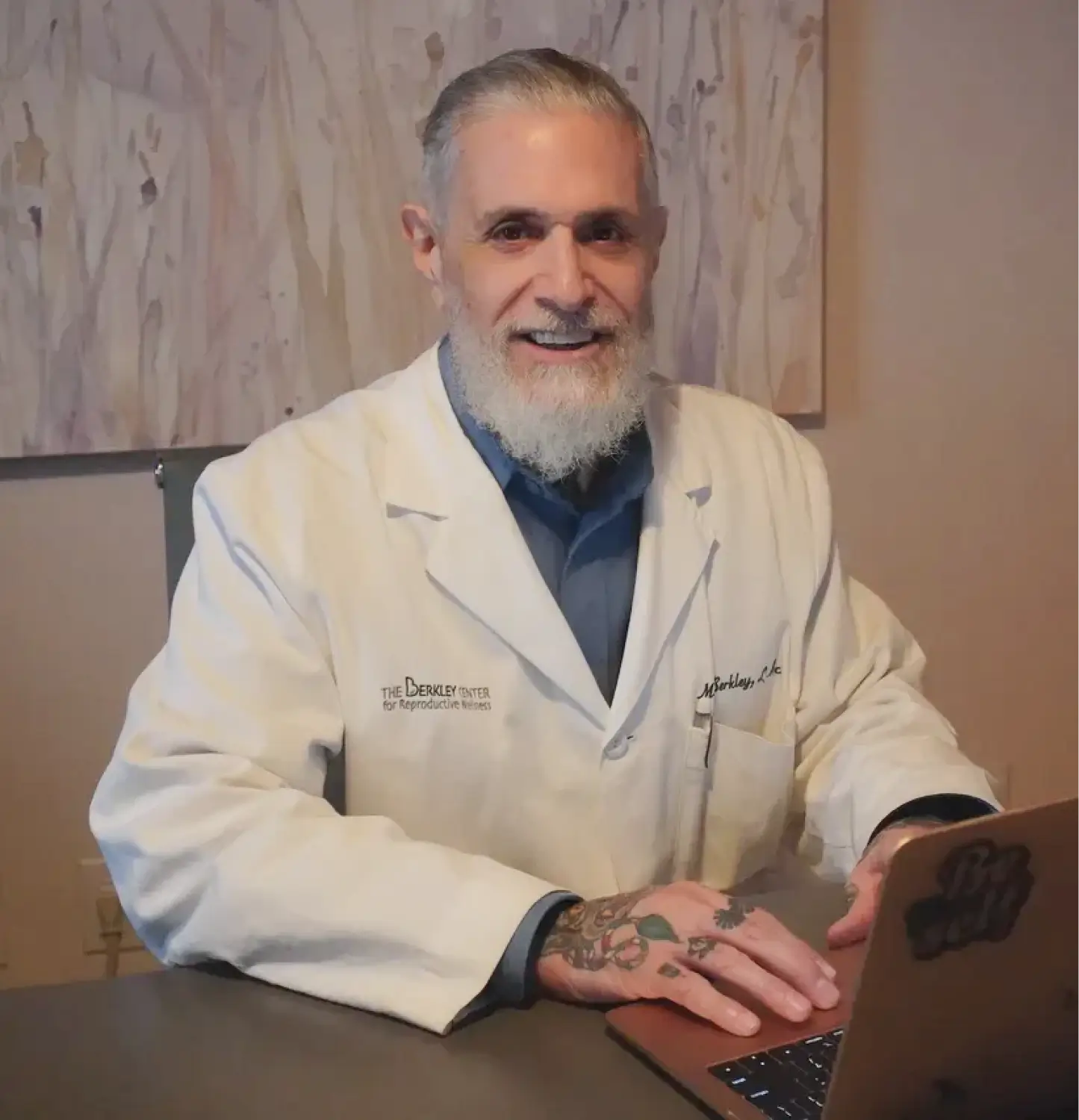
Mike Berkley, LAc, FABORM, is a licensed and board-certified acupuncturist and a board-certified herbalist. He is a fertility specialist at The Berkley Center for Reproductive Wellness in the Midtown East neighborhood of Manhattan, New York.
View all posts